Reflux Disease
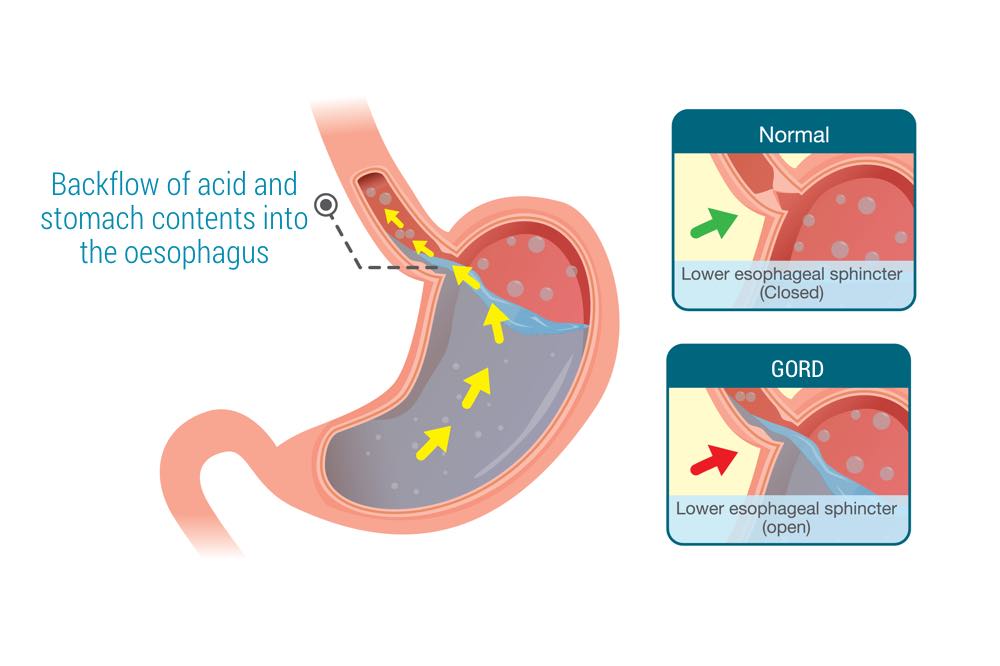
Gastro-Oesophageal Reflux Disease or GORD occurs when the stomach content flows back upwards into the oesophagus (also called the gullet or food pipe) causing irritation and inflammation to its inner lining (mucosa).
What is reflux disease?
GORD occurs when the stomach content flows back upwards into the oesophagus (also called the gullet or food pipe) causing irritation and inflammation to its inner lining (mucosa). This leads to symptoms most patients describe as:
- a burning sensation (heartburn) in the upper abdomen, radiating to the breast bone (and sometimes experienced as chest pain)
- regurgitation of gastric juices
- excessive belching
- stomach fluid content flowing all the way to the throat or aspirating down into lungs causing chronic coughing, wheezing or sore throat, as “atypical” symptoms in more severe cases.
At The Surgeons Collective, our team of top surgeons and medical staff are totally committed to delivering excellent outcomes, when we arrange your personalised care plan for benign gastro-oesophageal disorders. Throughout your treatment, our whole team will be by your side to support you and to provide an excellent care experience.
About Us
At The Surgeons Collective we work as a team of expert surgeons, as well as hepatologists, gastro-enterologists and accredited dietitians.
Benign oesophageal disorders
What causes Gastro-Oesophageal Reflux Disease (GORD)?
Gastro-Oesophageal Reflux disease (GORD) happens when a “valve” between your oesophagus and your stomach is impaired causing heartburn. For example, a hiatal hernia may cause the stomach to slip upwards in the chest, which causes interference with the valve, and this is how stomach acid fluid content flows back up in the oesophagus, causing heartburn.
GORD or Reflux Disease is usually diagnosed based on typical reflux symptoms. A trial of anti-acid medications can be used to confirm the diagnosis. If your diagnosis is unclear, or if you experience difficulty swallowing, vomiting or blood in stools, then an upper GI endoscopy can be performed. This is mostly to understand the underlying causes of the reflux and to exclude cancer.

If you have had a long standing history of GORD, the endoscopy also checks for complications such as:
- Oesophagitis: Inflammation of the inner lining of the food pipe due to long standing reflux. In severe cases, this could also lead to “ulceration” (shedding of the most superficial layer of the mucosa)
- Stricture: Narrowing of the lower portion of the oesophagus due to ongoing cycles of chronic inflammation from acid reflux injury and healing of the tissue by formation of scar tissue. This increasing accumulation of such scar tissue ultimately leads to progressive narrowing of the lumen of the food pipe which results in having difficulties swallowing (dysphagia).
- Barrett’s Oesophagus: This condition is often associated with GORD, whereby abnormal cells are found in the inner lining (mucosa). If that is the case, a small but significant risk of cancer (oesophageal adenocarcinoma) exists. This could be identified at the time of endoscopy and biopsies of these abnormal tissues are then examined under a microscope to confirm.
- Hiatal hernia: Check a more detailed description.
Another common test organised by your surgeon includes an oesophageal pH and manometry study. It involves placing a small, thin flexible tube with a specialised sensor into the oesophagus via the nostrils. Its main purpose is to confirm and measure the degree of acid reflux and also to rule out uncommon oesophageal dysmotility conditions (abnormal food pipe muscle contractions or “peristalsis”). This is vital to define the exact course of treatment.
If your GP has suggested that you may suffer from a Benign Oesophageal Disorder, it is important to consult with a specialist surgeon, who will define the most suitable treatment. At The Surgeons Collective Perth we combine the experience of 3 of Perth’s leading surgeons, and the expertise of our dietitians. It’s our mission to provide excellence in surgical and clinical outcomes, and to give you a comprehensive and clear diagnosis, as well as genuine care and support.
Quite often, the reflux symptoms will not require surgery, and will disappear with lifestyle changes or in combination with anti-acid drugs known as “Proton-pump inhibitors” ( e.g. Somac, Nexium, Losec, Pariet).
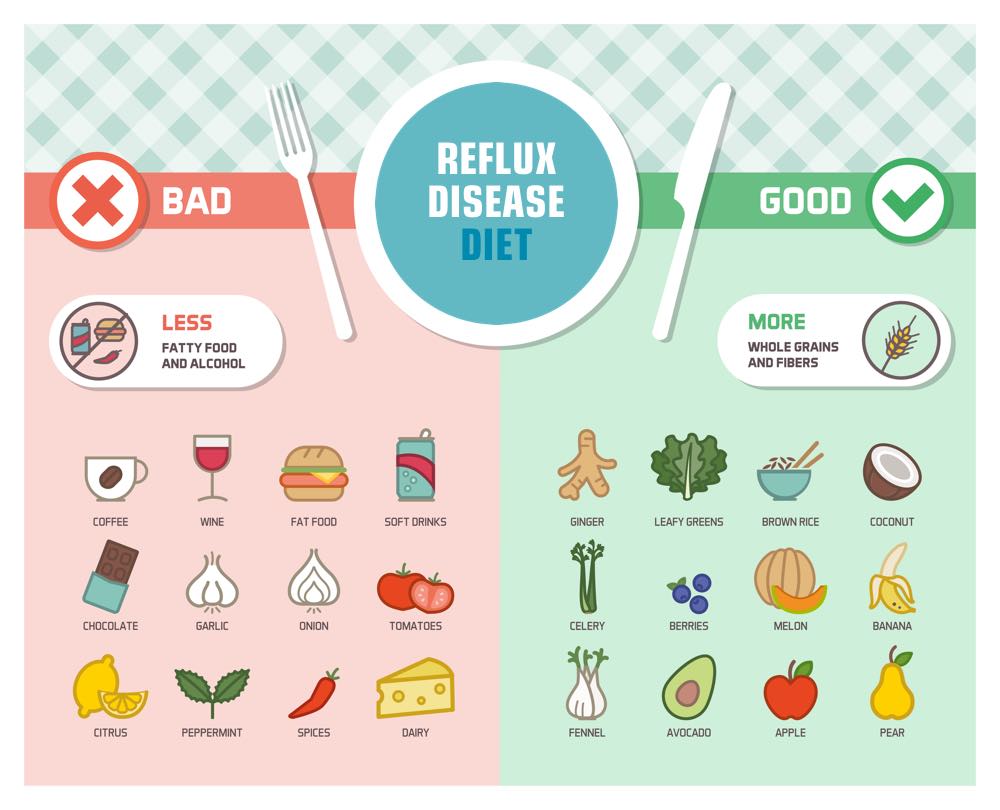
Lifestyle changes generally include:
- A change of diet: avoiding coffee, fizzy drinks, spicy or fatty foods and chocolate
- Reducing your alcohol intake
- Reducing your food portion sizes
- Avoiding late night meals and snacking
- Changing your head position when you sleep, changing the position of the oesophagus and using an extra pillow
- Losing weight
When do I need surgery for GORD or reflux disease?
Surgery for Reflux Disease may be required if:
- The reflux symptoms are not improved or relieved by maximal medical therapy
- You suffer from complications as a result of reflux
- Reflux causes respiratory complications
- You have a hiatal hernia
- There is a concern about the long term risks of using PPI medications.
Your specialist at The Surgeons Collective will make a careful assessment to determine the best possible treatment pathway. As a team, we commit to providing you with the best possible care experience, before, during and after your operation.
A “Laparoscopic Fundoplication” is a procedure which creates a well balanced “valve”, preventing acid from refluxing back upward, whilst allowing swallowed food to pass through into your stomach. In carefully selected patients, this operation is highly successful in alleviating a patient’s reflux symptoms and avoiding the need for long term use of anti-acid medications. Your surgeon will clarify this in greater detail when your diagnosis is discussed.
What diet applies for reflux disease?
Making dietary changes may help to manage your reflux. Reflux is often associated with being overweight or obese. Typical dietary changes that may help include avoiding carbonated beverages, avoiding alcohol, and limiting spicy, acidic, fatty foods, caffeine and chocolate. It may also help to have smaller frequent meals and not to eat within 2 hours of going to bed.
Contact us
THE SURGEONS COLLECTIVE
McCourt St Medical Centre
Level 1, Suite 10, 2 McCourt Street
West Leederville,
Perth 6007, WA
THE SURGEONS COLLECTIVE
Monday - Thursday | 8:30am - 4:30pm
Friday | 9:00am - 1:30pm